I wanted to share just part of my ongoing journey of being diagnosed. I say ongoing, because this crap is never ending. I won’t go into much detail on my symptoms or specifics on bad days, just because it is so much that my son and husband might start thinking I have abandoned them. I will do weekly post about current hard days and symptoms and maybe more specifics at a later time.
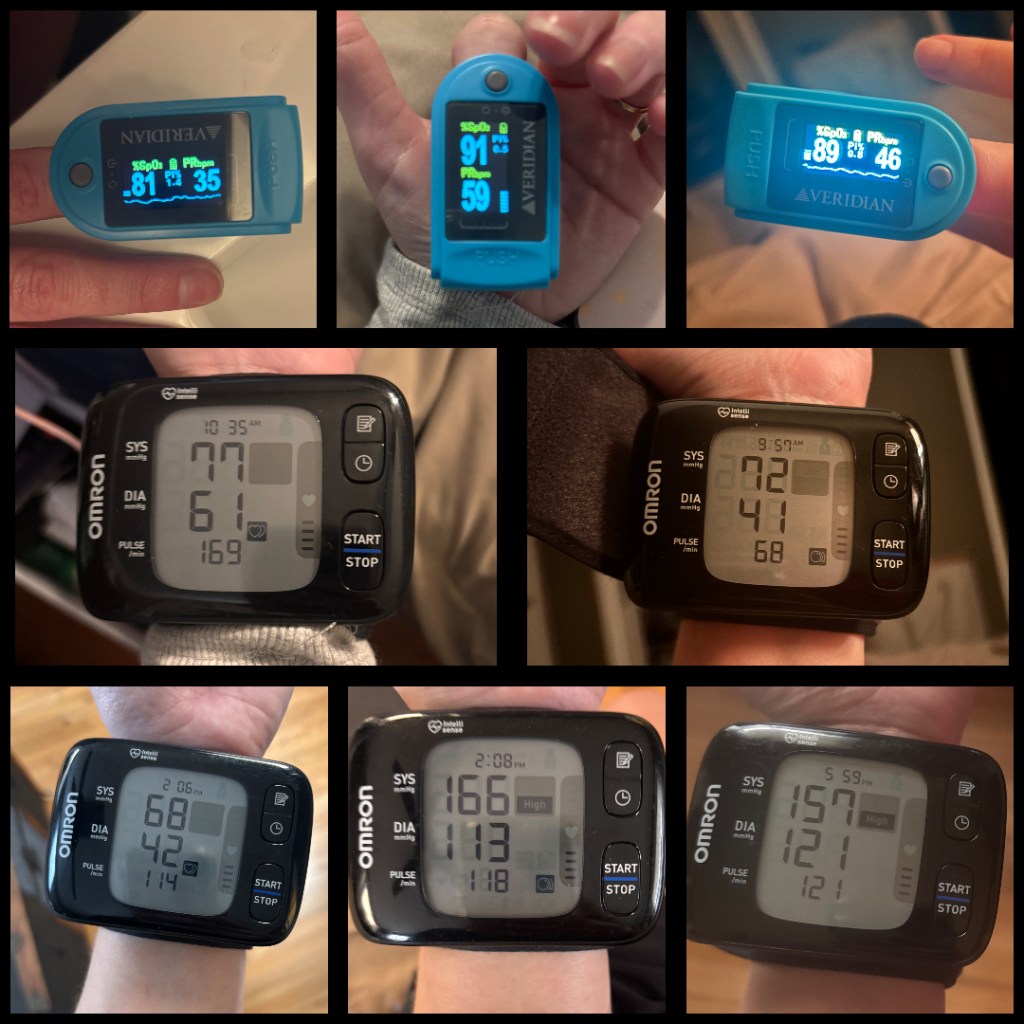
April 2024 I started getting sick. I was throwing up all the time, losing weight (let’s be real, I needed to lose some weight anyway), having GI issues, difficulty swallowing food, but the big thing was I would pass out literally every single time I stood up and walked more than about five feet. I spent the next two months going to the Doctor and being a human pin cushion. I cannot even guess the number of test that I had, but of course most things came back normal (I say most, but since I was also having food issues, my labs were all abnormally normal). One night I couldn’t stop throwing up, I just felt awful in general, and my husband couldn’t watch anymore, so he made me go to the hospital. At the hospital my blood pressure was so low, they kept retaking it thinking that something was reading wrong. Long story short I was admitted and it was suggested that I get the gastric emptying test done because they were thinking it was gastroparesis……which it was. I just didn’t realize that it was more than that. I tried every medicine under the sun and even some from out of the country (chill…it was still Doctor recommended and prescribed), but nothing worked. I was also put on midodrine for low blood pressure.
Things seemed to level out for a while. I left my job for my dream job, and I felt on top of the world. Of course, the lifestyle changes I had to make for the gastroparesis sucked, but I was happy. My marriage was great, my son was great, my job was freaking awesome. But in February 2025, I started getting sick again. I’ll spare you the symptoms because let’s be real, it’s too many to list anyway. At the beginning of March 2025, I had to take a leave from work, I ended up in the hospital again and things were just bad (at least at the time I thought they were bad). I went through months of doctor appointments, tests, being practically bed bound and things just got worse each month. I eventually had to resign from work because it was clear I would not be well enough to return anytime soon anyway. I finally had a doctor tell me that they thought it could be POTS, but most people around here don’t test for it because there is no cure anyway (yes, that was what she said). I was finally able to find a Cardiologist who diagnosis it, and after a 6 month wait, she gave me this diagnosis: somatoform autonomic dysfunction: a combination of inappropriate sinus tachycardia, POTS, orthostatic hypotension, on top of my gastroparesis.